In the realm of healthcare, technology plays a crucial role in streamlining operations and improving patient outcomes. ehr software development is at the forefront of this transformation, offering healthcare professionals a way to manage patient data, medical histories, and treatment plans more efficiently. However, as vital as EHR systems are, their success depends heavily on user experience (UX) design. A well-designed EHR system can enhance productivity, reduce errors, and provide a seamless experience for both healthcare providers and patients.
This article delves into the best practices for developers to create user-friendly EHR software, emphasizing the critical role of UX design in healthcare technology.
Understanding EHR and the Importance of UX Design
Electronic Health Records (EHRs) are digital versions of a patient's medical history, maintained over time by the healthcare provider. These records may include all of the key administrative clinical data relevant to that patient, such as demographics, progress notes, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports.
While EHR systems provide numerous benefits, such as improving healthcare coordination, reducing medical errors, and increasing productivity, their complexity can also create challenges. Poorly designed EHR interfaces can frustrate users, leading to increased cognitive load, inefficiency, and even medical errors.
Here’s why UX design in EHR software is essential:
- Improved Efficiency: Well-designed EHR systems allow healthcare professionals to access the information they need quickly and easily, reducing the time spent on administrative tasks.
- Reduced Errors: A clear and intuitive design reduces the likelihood of errors in patient data entry or treatment management.
- Better Patient Outcomes: By making it easier for clinicians to track patient information, a well-designed EHR can contribute to improved patient outcomes.
- Enhanced User Satisfaction: A system that is easy to navigate and aligns with the user’s workflow increases overall satisfaction and reduces frustration.
The core principle behind UX design in EHR software is creating a user-centric system. This means designing an interface that aligns with the actual needs, workflows, and preferences of its users, primarily healthcare professionals.
Best Practices for UX Design in EHR Software
1. User-Centered Design (UCD)
User-centered design is a methodology that places the end-user at the heart of the development process. For EHR systems, this involves understanding the workflows and needs of healthcare professionals, such as doctors, nurses, and administrative staff, and then designing the system to meet those needs.
Key steps in implementing UCD include:
- User Research: Before designing the system, conduct thorough research to understand how different healthcare providers use EHR systems. This could involve interviews, surveys, and direct observation of their workflows.
- Personas and Scenarios: Create user personas to represent different types of users (e.g., physicians, nurses, administrators) and scenarios to understand how they interact with the EHR in various situations.
- Iterative Design and Testing: Develop prototypes and test them with real users to get feedback. This iterative process ensures that the design is refined and optimized according to actual user feedback.
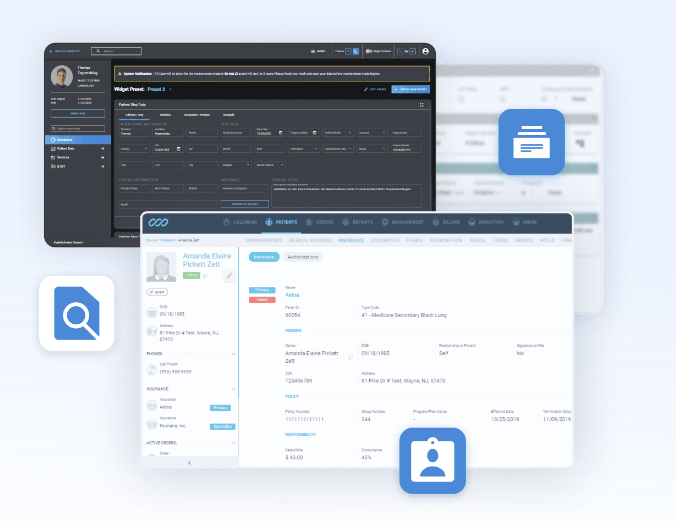
2. Simplifying the Interface
EHR systems handle a vast amount of information, which can easily overwhelm users if the interface is cluttered. A key principle of UX design is to keep the interface simple and uncluttered, allowing users to focus on essential tasks without unnecessary distractions.
- Prioritize Information: Not all data is equally important. Use hierarchy and organization to prioritize the most critical information (e.g., vital signs, medication lists) at the top, while less urgent information can be available through secondary screens.
- Clear Navigation: The navigation system should be intuitive and consistent, allowing users to find what they need quickly without having to memorize complex pathways.
- Minimalist Design: Avoid cluttering the screen with too much information. Use white space strategically to make the interface less overwhelming, and ensure that all elements serve a clear purpose.
3. Streamlining Workflows
One of the primary reasons for adopting EHR systems is to improve the efficiency of healthcare workflows. A poorly designed EHR system can complicate rather than streamline these workflows, making it harder for healthcare professionals to do their jobs.
To optimize workflows in EHR software:
- Mapping Current Workflows: Conduct a thorough analysis of the current workflows of healthcare providers to identify bottlenecks and inefficiencies. Design the EHR system to align with these workflows, rather than forcing users to adapt to a new one.
- Automation and Integration: Automate repetitive tasks (e.g., billing, appointment scheduling) to save time and reduce errors. Ensure that the EHR system integrates with other healthcare systems (e.g., laboratory systems, radiology systems) so that users don’t have to switch between different platforms.
- Customizable Dashboards: Allow users to customize their dashboards according to their preferences and needs. For example, a nurse might want quick access to vital signs and medication lists, while a physician might prioritize diagnostic results.
4. Minimizing Cognitive Load
Healthcare providers often work in high-pressure environments where they must process vast amounts of information quickly. EHR systems should be designed to minimize cognitive load, reducing the mental effort required to complete tasks.
- Consistency: Consistent design patterns (e.g., button placement, font styles, and icons) help users learn the system faster and avoid confusion.
- Visual Hierarchy: Use visual cues, such as size, color, and positioning, to create a clear hierarchy of information. For example, use bold fonts and larger sizes for important patient details like allergies or critical lab results.
- Progressive Disclosure: Show only the necessary information on each screen, allowing users to reveal more detailed information as needed. This approach prevents information overload and keeps the user focused on the task at hand.
5. Ensuring Accessibility
Accessibility is a fundamental aspect of UX design in EHR systems. Healthcare professionals come from diverse backgrounds, with varying levels of technical proficiency and potential physical limitations. An accessible EHR ensures that all users, including those with disabilities, can use the system effectively.
- Keyboard Navigation: Ensure that all actions can be performed using keyboard shortcuts, which can be faster and more efficient than using a mouse for some users.
- Screen Reader Compatibility: EHR systems should be compatible with screen readers to support users with visual impairments.
- Color Contrast: Use high contrast between text and background colors to improve readability, particularly for users with visual impairments or color blindness.
- Font Size Adjustability: Allow users to adjust the font size to suit their preferences or needs, ensuring that the interface is legible for all.
6. Providing Real-Time Feedback
Real-time feedback is crucial for ensuring that users understand the consequences of their actions within the EHR system. Feedback helps users confirm that the system has processed their input correctly, reducing uncertainty and potential errors.
- Confirmation Messages: Provide clear confirmation messages when users complete important tasks, such as saving a patient’s record or sending a prescription.
- Error Prevention and Recovery: Use feedback mechanisms to prevent errors, such as warning messages when a required field is left empty. Also, provide clear instructions on how to recover from errors.
- Loading Indicators: When the system is processing information, use loading indicators to inform the user that the system is working, reducing the likelihood of multiple clicks or actions.
7. Ensuring Data Security and Privacy
EHR systems handle sensitive patient information, so data security and privacy are paramount. However, security measures should not compromise usability. Balancing these two factors is a key challenge for UX designers.
- Role-Based Access Control: Implement role-based access control (RBAC) to ensure that users can only access information relevant to their role. For example, a nurse might have access to different information than a physician or administrative staff.
- Easy-to-Understand Privacy Policies: Clearly explain the system’s privacy policies to users, ensuring that they understand how patient data is protected.
- Seamless Authentication: Use multi-factor authentication (MFA) and single sign-on (SSO) to improve security without creating a cumbersome login process.
8. Supporting Mobile and Tablet Use
Healthcare providers are often on the move, whether they are rounding in a hospital or visiting patients in outpatient settings. EHR systems must be optimized for mobile and tablet use, allowing healthcare professionals to access patient data wherever they are.
- Responsive Design: Design the EHR system to be responsive, ensuring that it works well on both desktop computers and mobile devices.
- Touch-Friendly Interfaces: Ensure that the interface is touch-friendly, with large buttons and easy navigation, making it simple to use on tablets and smartphones.
- Offline Access: In cases where internet connectivity is an issue, the EHR system should allow offline access to critical patient information, with the ability to sync when back online.
9. Ensuring Interoperability
EHR systems rarely operate in isolation; they need to communicate with other healthcare systems, such as laboratory information systems, pharmacy systems, and radiology systems. Ensuring interoperability is critical for improving the overall UX of an EHR system.
- Open APIs: Use open application programming interfaces (APIs) to facilitate data exchange between different systems, ensuring that users can access all the information they need without switching between platforms.
- Standardized Data Formats: Adopt standardized data formats, such as HL7 or FHIR, to ensure that data can be shared and interpreted correctly between different systems.